Billing Solutions
We are small billing company that company specially designed to serve individual to small group practices (Medical and Mental Health).
The rate we charge is a percentage of the total amount on collected (paid) claims only, or on a per claim basis (including rejected claims – meaning front end of the billing cycle issues such us no coverage, pre-authorization, plan c issues for Medicare, etc).
Utilizing our own resources, our service covers the cost of the billing software, the clearinghouse and all necessary expenses to submit the claims electronically, thus allowing the Practitioners to focus on patient/client care.
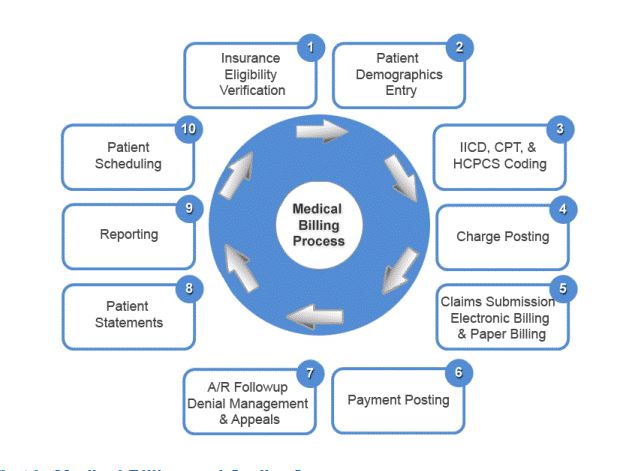
Once an agreement is reached – We give our clients options on how to work together. For example, if you prefer to have us utilize your existing EMR Software in order to process your claims, you would simply provide us with a report from your EMR on charts that are ready for billing and the log in information. We would then review your patients’ charts and assign the corresponding level of Evaluation and Management CPT codes, in accordance with the E/M Guideline and CPT codes for other procedures. This includes assigning the ICD 10 diagnosis codes. Alternatively, we can provide a superbill for your Practice to fill out and send to us via e-mail/fax. Once the claims are processed, We send a detailed report for your records. Please note – for Payors that do not require EDI enrollment – claims will be processed as soon as possible. For local clients, per your preference– we could also work in your office location – thus earning our nickname — “The Portable Biller”.
Most importantly, our turnover is 24 to 48 hours, depending on the number of claims. For example, if we receive 50 claims today, the claims will be submitted by the next business day. For over 100 claims, usually our turnover is 48 hours.
In addition to billing, oftentimes Solo Practitioners would want to add insurance panels to their practice. Therefore, another time-consuming task is necessary to achieve this goal. We charge a flat rate of $250.00 for credentialing per insurance panel. Finally– for maintenance purposes (revalidation-re-attestation) of already credentialed Providers – this service is free.
Choosing to outsource your billing or switch to a new billing company is an IMPORTANT investment decision. We know that this decision can be very difficult. What separates us from our competition is our flexibility to meet your billing needs. We do understand how busy your schedule can be. But, if you find any free time, please do not hesitate to contact us any time..